For Medical Professionals
About HBOT
Understanding the role of oxygen in the human body is essential to a full comprehension of what frequently causes cerebral palsy and the many other off-label conditions that HBOT has shown to have a positive effect on; hyperbaric oxygenation can play an important role in decreasing, or even ameliorating, the effects of cerebral palsy and brain injuries, stroke, concussions, and arthritis. Until one understands the effect of oxygen on the body, especially the brain, it can be difficult to see the relationship between hyperbaric oxygen therapy and cerebral palsy, or to discern how increasing the oxygen pressure in blood flowing to the brain can be of benefit in decreasing the symptoms of CP and many other conditions.
Oxygen availability within the body
When oxygen is appropriately available to the critical parts of the body (the brain, heart, and lungs), it can mean the difference between life and death, coma and mental alertness, paralysis and movement, illness and health. When a portion of the brain is deprived of the correct amount of oxygen, any or all of the above conditions, as well as other impairments, may take place.
Oxygen is carried throughout the body by red blood cells, which contain the binding factor hemoglobin. When oxygen is inhaled, the molecules dissolve in plasma and bind to the hemoglobin of red blood cells, which in turn carry oxygen to the body’s tissues – all tissues, not just brain tissues. Once oxygen has been transferred into the tissue, it is replaced with carbon dioxide (as waste product) that also binds to hemoglobin and is transported to the lungs where it is discharged. Thus, the delivery of oxygen under normal physiological circumstances requires appropriate circulation and is energy dependent at the cellular level.
Hyperbaric conditions
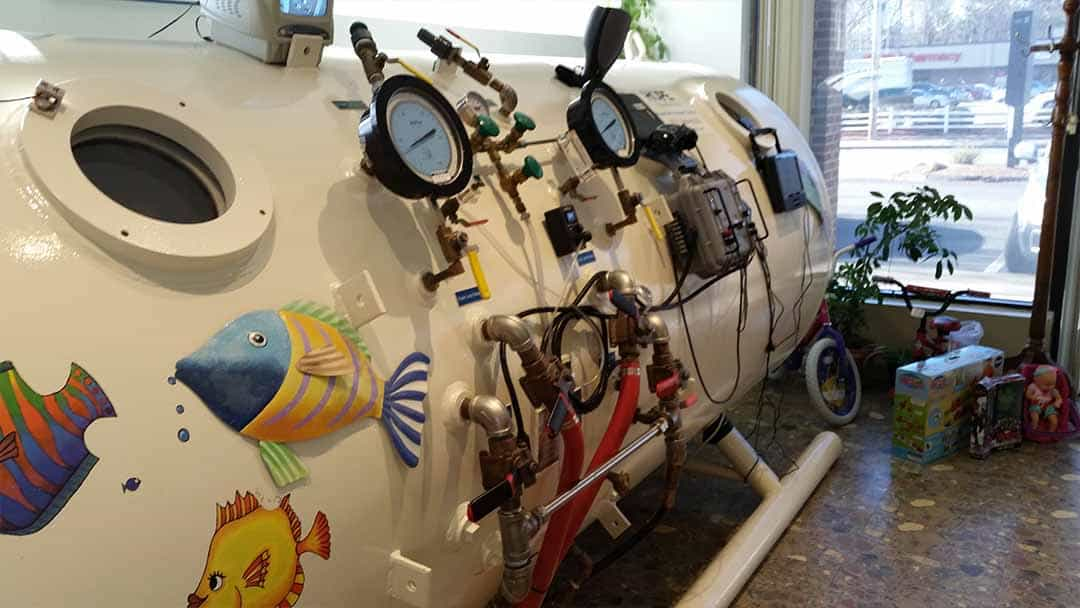
Under conditions of hyperbaric oxygen, patients breathe 100% oxygen in a pressurized chamber; this oxygen is the same gas that the body uses naturally without being under pressure. Under pressure there is increased penetration into tissues of the body. Oxygen under pressure will dissolve into body tissue and fluids in a direct proportion to the pressure used (Henry’s gas law of physics). Oxygen is thereby dissolved in the plasma, cells, bone, urine, blood, muscles, etc., and most importantly, cerebral spinal fluid.
This explains the significance of the statement by Edward Teller, Ph.D.,* that “hyperbaric oxygen delivers free molecular oxygen at the tissue level for immediate metabolic use without any energy exchange, even when the circulation is impaired.”
In animal studies conducted by Dr. Ite Boerema, a Dutch physician, it was proven that hyperbaric oxygen can supply adequate amounts of oxygen to all organs of the body, even without blood. Under hyperbaric conditions, he replaced the blood circulating through pigs’ bodies with saline solution. There was enough oxygen dissolved in other fluids of the body that the animals survived without any interruption of vital functions. Hemoglobin, carried by the red blood cells, is essential for the normal transport of oxygen, but from the standpoint of being the essential delivery system, it may be bypassed, at least on a temporary basis, if there is sufficient oxygen in the body fluids.
Normal conditions
Under normal circumstances, the required oxygen flows through the body to the various parts (heart, lungs, stomach (home to 100 trillion bacterial cells), brain, etc.) via the circulatory system. If there is any type of interruption of blood flow, it means that the amount of available oxygen, down to the capillaries and the tissues, may be seriously reduced. When the arterial flow is hindered, ischemia (loss of blood flow) and hypoxia (lack of oxygen) are the results.
Equally important, oxygen flowing through the blood brings about certain chemical reactions within the body that result in energy production. Energy is required for circulation, respiration, digestion, maintaining constant body temperature, and proper brain function. Only a minute amount of oxygen is required for normal intracellular chemical reactions to take place, and under normal circumstances, the rate of oxygen used is determined by the rate at which the respective cells expend energy. Energy production, aided by oxygen, is vitally important in the brain where the cells need adequate energy to generate the electrical activity that causes it to function properly.
Oxygen deficient cell viability
Thus, oxygen is a critical element in the functioning of all parts of the body. If cells do not receive any oxygen, they die and may not be regenerated. On the other hand, if a cell is getting a small amount of oxygen, it can remain viable for a much longer period than previously thought. In the case of a child with cerebral palsy or traumatic brain injury, for example, we are primarily interested in the brain cells (neurons), the length of time they remain viable, and how they can be revitalized.
It is important to remember that the same facts regarding the need for oxygen to sustain life, and the time some cells may remain viable, are as true of neurons as any other cell in the body. The critical issue to remember when discussing cerebral palsy and other brain injuries is that if the mitochondria of certain cells do not receive enough oxygen to operate properly, but are receiving some oxygen, they may not die. In this hypoxia (under oxygenation of the tissues) occurs. It was scientifically proven in the mid-1980s that dormant brain cells can remain viable for many years. In the meantime, however, the diminished supply of oxygen causes multiple symptoms such as mental disturbances, shortness of breath, rapid pulse, fall in blood pressure, and, if there is a severe loss of oxygen, cyanosis (blueness of the skin and mucous membranes).
Decompression illness and air pressure treatment
The knowledge that hyperbaric oxygen treatment has a value to the body is not altogether new. Increased air pressure has been used for over a hundred years by the diving community to alleviate diving-related illnesses. The first actual use of air under pressure to treat decompression illness was in 1848. Although those who used this pressurized air did not know it, the compressed air naturally boosted the oxygen content of the plasma.
Today, it is common practice to use oxygen, administered in a hyperbaric chamber for multiple sclerosis (MS), Lyme disease, reflex sympathetic dystrophy (RSD), and many other disabling neurological and auto-immune conditions.
To the majority in the medical profession, hyperbaric oxygen therapy is a relatively new therapy for young children and adults. HBOT is simply the delivery of 100% pure oxygen at greater than atmospheric pressure through the use of a hyperbaric chamber. [This is referred to as ATA (absolute atmospheres) in discussing hyperbaric oxygen therapy.] The pressure can be administered in ranges from 1.1 to 3 ATA using 100% oxygen. Even lower pressures may be needed if seizure activity is present. Under these circumstances, pressures of 1.1 to 1.25 ATA using 100 percent oxygen are appropriate. This frequently treats the seizure disorder and thereby helps to reduce or stop ancillary medications.
Applications of HBOT
Physicians in the US and abroad have increasing opportunities to experience first-hand the benefits of HBOT on MS, age-related macular degeneration, acquired (and other) immune deficiencies, Lyme disease, cerebral palsy, and brain injuries. Studies from around the world are currently yielding impressive results demonstrating that reactivating dormant brain cells with HBOT can have positive effects on many types of brain injuries.
Success of hyperbaric oxygen in any given case is dependent upon the location and extent of the irreparable damage and the location and extent of the potentially recoverable areas of the insult, overall physical condition, and/or severity of the patient’s injury. While not necessarily a cure, hyperbaric oxygen offers the best chance of recovery for patients suffering from a variety of medical conditions.
When administered properly by trained medical personnel, HBOT causes no pain or discomfort and is completely non-invasive. At the same time, we encourage caregivers and medical personnel to fully investigate our facility before using it or recommending our service.
* Dr. Teller developed the hydrogen bomb.

Helpful Links – Orgs & Lit
Organizations
- American College for Advancement in Medicine (ACAM), for physicians and medical professionals interested in the latest in integrative and complementary medicine, including HBOT.
- Holistic Dental Network, where patients, consumers, and Holistic professionals meet. You will find the answers to your questions about mercury toxicity, dental amalgam health problems, heavy metal body burden, biocompatibility of composite dental restorations, nonmetallic and non-mercury filings, protocols for mercury amalgam removal, as well as biological microscopic non-surgical gum care.
- UHMS, Undersea and Hyperbaric Medical Society, is an international, non-profit organization serving over 2,400 members from more than 50 countries. The UHMS is the primary source of scientific information for diving and hyperbaric medicine physiology worldwide.
- ARI, Autism Research Institute, a non-profit research, resource, and referral organization that conducts and funds research that makes a difference in finding the causes and developing safe, effective treatments for autism.
- MUMS, a national Parent-to-Parent organization for parents or care providers of a child with any disability, rare or not so rare disorder, chromosomal abnormality or health condition. A must-see for anyone involved in the medical community.
- (lyme) Lyme disease resources.
- MDA Resource links, by state.
- MDA Research News, current and updated.
- Major medical research links and clinical trials (non-HBOT specific), provided by the MDA and including ALS and genetic testing links.
- WAPF, a central meeting point for health care professionals who use Weston A. Price’s nutritional principles in their practice.
- Wound Healing Society, for wound healing basic and clinical scientists and wound care practitioners to keep pace with the rapid developments in the interdisciplinary field of wound healing research.
- Courses in hyperbaric medicine, by UHMS.
Books
- Best Publishing, the premiere hyperbaric medicine and HBOT publisher.
- Hyperbaric Oxygen Therapy, by Neubauer, M.D. and Walker, M.D.. Highly recommended. (free preview)
- Hyperbaric Oxygenation for Cerebral Palsy and the Brain Injured Child: A Promising Treatment, by Neubauer, M.D. If you should have read one book on hyperbaric oxygen, this is it!
- The Oxygen Revolution: Hyperbaric Oxygen Therapy: The Groundbreaking New Treatment for Stroke, Alzheimer’s, Parkinson’s, Arthritis, Autism, Learning Disabilities and More, by Harch, M.D. (free preview)
- Hyperbaric Medicine Practice, by Kindwall, M.D. and Whelan, M.D. (free preview)
- Physiology and Medicine of Hyperbaric Oxygen Therapy, Neuman, M.D. and Thom, M.D. (free preview)
- Hyperbaric Nursing, by Larson-Lohr and Novell. (free preview)
- (lyme) Lyme Times periodical
Studies
- HBOT and drug interactions, links to studies and articles (collected and hosted by Rubicon Research Repository).
- Oxygen toxicity and HBOT, links to studies and articles (collected and hosted by Rubicon Research Repository).
- (lyme) Lyme Disease Medical Literature Summaries (LymeInfo.net)
- Hyperbaric Oxygen UK, providing a wealth of information about HBOT, including studies not readily available in the US.
Articles
- Prevention of middle ear barotrauma, online article by Edmond Kay, M.D.
- Johns Hopkins Medicine general overview of HBOT.
- BMC Complementary and Alternative Medicine is an open access, peer-reviewed journal that considers articles on interventions and resources that complement or replace conventional therapies, with a specific emphasis on research that explores the biological mechanisms of action, as well as their efficacy, safety, costs, patterns of use and/or implementation.
See Facebook page for full list
FAQs for Medical Professionals
Hyperbaric oxygen as it applies to brain injury
HBO is a therapeutic modality that reduces cerebral edema (acute or long-term swelling) and improves the functions of the brain’s (or any other organ’s) tissues (called neurons in the brain) that have been rendered inactive by ischemia/hypoxia (deficiency of oxygen) by giving 100% oxygen under pressure in a hyperbaric chamber. The improvement of brain function, specifically, is reflected by the improved electrical activity of the brain. In other words, hyperbaric oxygen (HBO) uses pure oxygen under pressure to speed and enhance the body’s natural ability to heal. While often used as a primary emergency treatment (for example, in an ambulance on the way to the hospital), it is more often used as a cost-effective adjunct of enhancement therapy for patients who suffer from various diseases or conditions (mitochondrial, Lyme, RSD, Lupus, fibromyalgia, and autism, to name a few) or injuries associated with hypoxia (lack of oxygen) on a cellular level. It is at this cellular level where all life processes take place.
HBO research in the United States
HBO is still considered an alternative therapy in the US. It will remain in this alternative status until controlled, double-blind studies are conducted. In other countries, it is possible to do controlled studies with funding provided by the government. In the United States, most of the funding for neurological studies, for example, is regulated by the National Institute of Neurological Disorders and Strokes (NINDS), operated under the auspices of the US Department of Health and Human Services (part of the National Institutes of Health). The cost of controlled, double-blind studies in the US is approximately $250,000 each. In addition, studies on new procedures, medications, or protocols are usually funded in the US by pharmaceutical companies where profit must be the primary focus. Pressurized oxygen is not a “drug” that pharmaceutical companies find financially advantageous. Finally, most medical schools do not have courses on hyperbaric oxygen. This lack of training does not give the average physician a comprehensive understanding of hyperbarics or the knowledge needed to assist caregivers to make an informed decision about its use.
HBOT for cerebral palsy
The National Institute of Health in the United Kingdom pays for treatments for children with cerebral palsy, but in the US the majority of insurance companies do not typically pay for treatments that have not been formally approved by either Medicare or the AMA. There are some progressive companies that have begun to cover HBOT for the brain-injured child, but as long as HBOT for cerebral palsy is considered alternative, costs will remain the responsibility of the caregiver. On the positive side, most major insurance companies will pay for the medical evaluation of the child, including the SPECT scans, both for diagnostic purposes to begin HBOT and subsequent scans to document improvement to brain function as well as concomitant therapies.
HBOT for children
By including not only the rationale of HBOT, but also its history, pertinent research, and physiological effects of oxygen on the body, specifically on the brain, it is hoped that caregivers will feel more confident about making their own decisions about the value of hyperbaric oxygen therapy for their child. It is important for the caregiver to remember that like any other form of therapy, HBOT is not intended to be the exclusive treatment used in cases of children with, say, cerebral palsy or brain injuries. Rather, it is recommended that it be part of the overall plan to help the child obtain as much independence and normal body function as possible. It is further hoped that members of the healthcare team, including physical, occupational, and speech therapists, will view HBOT as an ally to the individual child’s plan of care. At HOPE, we believe that caregivers should have access to the information they need to talk objectively to their own physician and care-giving team about this treatment modality.
Does HBOT help every child?
Unfortunately, it does not. As with any medical intervention, there are some children who do not seem to improve significantly with hyperbaric oxygen. For the most part, however, there is an 80%-90% correlation between changes on the SPECT scan and noticeable improvement. Usually, this improvement can be determined before the child completes the initial 40 hours of HBOT, but not always. Occasionally, even when there is not much change on the SPECT scans as the first series of treatments are concluding, parents do notice significant improvements later on. When the only change in the child’s medical plan is hyperbaric oxygen, it is difficult to discount the value of HBOT. This is why each child must act as his or her own control.
How soon will results appear for the brain-inured child?
This is a frequently asked question but difficult to answer. We do not always see immediate improvements in children with cerebral palsy, but we do see rapid improvement in children with brain injuries. This is especially true if we treat the child soon after the brain damage occurs. In short, the sooner HBOT is started, the better the results. This often applies to the speed of improvements as well.; the sooner the HBOT is started after a brain injury of any type, the sooner improvements are observed. It appears that the longer the time that elapses before HBOT is started, the longer it takes to see improvement and, to some degree, less improvement is seen. Furthermore, Dr. K.K. Jain in his Textbook of Hyperbaric Medicinereports that “repetitive HBO appears to be trophic, stimulatory to brain repair, and may not be complete in some cases until 200-300 treatments.” Of course, each child is different, as is the extent of his or her brain damage and its specific location. All of these factors affect the extent and rapidity of improvement. Not all children see dramatic results. Sometimes the improvements are merely a decrease in the degree of spasticity, or the ability to hold a cup and drink with one hand rather than two hands. In other cases, the child is able to decrease or discontinue medication for seizures, or the frequency of seizures may diminish significantly. All of these improvements are important to the child and his or her caregiver but may be difficult for an outsider to distinguish or to document scientifically.
How many hours of HBOT are needed?
Because each person is unique, the number of HBOT sessions will vary. The actual number of hours needed will depend, in part, on age, health, speed of improvement, goal of treatments, caregivers’ time-frame, and financial means, etc. While each case is different, standard protocol is to give an initial series (40-80 hours in the case of cerebral palsy and brain injury client-patients) unless a different number is needed, depending on the reason for using HBOT. Each session will lsat approximately an hour, with the total session time starting from the moment that the chamber begins to be pressurized. Longer term conditionstake more time to correct. Some client-patients have had over 300 hours of HBOT with continuing improvement.
The HBO medical community
The community of doctors and nurses adopting HBOT on a day-to-day basis is growing rapidly. The growth in the medical community’s use of HBOT is due, largely, to organizations like the UHMS, the Society of Baromedical Nurses, and the incorporation, now, of hyperbaric chambers in most ambulance and first-responder vehicles, along with the growing evidence from studies and testimonies of caregivers and parents. The medical community owes a great deal to individuals who brought new ideas and procedures to the field of hyperbarics. These founders of modern hyperbaric medicine were willing to stand apart from their fellow physicians and scientists and declar their belief in air and oxygen therapy. To demonstrate their faith in HBOT, they used their ingenuity and intuition to design and construct chambers. They often suffered severe criticism from others and were ostracized by their fellow medical professionals. Clearly, without their belief in their own creative and innovative ideas, hyperbaric medicine might never have become available to so many of today’s illnesses and diseases.
What is a SPECT scan?
Single photon emission computed tomography (SPECT) scanning is a relatively new, advanced diagnostic nuclear medical imaging procedure that provides a “cross section” image of the body, similar to those generated by computerized tomography (CT), also known as computerized axial tomography (CAT). Its primary purpose is to determine blood flow in the various organs of the body. It is particularly beneficial in the study of the brain. Unlike MRI or CAT scans, whose purpose is to show the anatomy of the body, SPECT scans show actual body functions, including brain function. An infinitesimal amount of a short-lived radioactive tracer is injected into an individual’s bloodstream through the arm or any vein. It releases energy impulse, which are then identified by the sensitive detectors of the SPECT scanner. The radioisotope used for tracing brains has the ability to cross the blood-brain barrier, which allows the doctor to determine how blood is distributed through different parts of the brain and to visualize brain metabolism. The scans produced by the gamma camera give the doctor the means to distinguish between dead and living cells, to determine the effects of pre- and post-HBOT sessions, and to make a better diagnosis of the client-patient’s actual condition. SPECT is a non-confining, painless procedure and takes about 30-40 minutes. The initial scan of the brain gives a baseline report of its function. This is critical in making a correct diagnosis of the progress and value of hyperbaric oxygen. It is usually imperative that there be areas of the brain which show the ability to recover through the use of increased oxygen tension. I no idling brain cells (in the case of brain injury and cerebral palsy) are located, HBOT may not be helpful. There have been instances, however, when significant improvement has taken place in a patient in spite of the absence of visible recoverable neurons. Cases such as these may be evidence of the brain’s capacity for plasticity (the ability of one part of the brain to take over for another part), the basis for neuro-rehabilitation.
As a doctor, how can I learn more about HOPE Connection?
We encourage doctors in all specialties to learn more about HOPE Connection and HBOT. Our goal is not to influence decision-making but to work with medical professionals in understanding the history and application of HBOT to their practices. We can help with insights on operations, safety, and, of course, answers to questions on proper protocols for many conditions that HBOT has proven successful in combatting. We strive to educate any healthcare professional seeking information and speak with specialists in all areas on a weekly basis. Many individuals, whether caregivers, parents, or specialists, stumble across HBOT in their practice, and we often fill void between what’s ‘understood’ about HBOT and the reality of where HBOT is today. HBOT is being used in every state and in 98% of every hospital network around the country. As individuals make inquiries into HOPE, we learn more about the growing community of professionals adopting HBOT in their daily operations. No doubt, the medical professionals in the oxygenation arena are improving their understanding of HBOT and able to answer client-patient questions in a more informed manner. Through HOPE and this growing community, patients, educated parents, and caregivers are learning about the possibilities of HBOT through third-party studies and literature. We provide a safe, well-managed and regulated environment and encourage doctor participation. This site is an informational site only, but there are many doctors in the Boston and New England area that can offer real-world examples of HBOT success. Just let us know how we can facilitate the conversation. Email your questions to [email protected] or call the office.
As a nurse who works with stroke and TBI survivors, can you introduce me to HBOT?
The individuals at HOPE include certified home-health aides and EMTs who provided full care to a variety of individuals. There is a lot to learn about HBOT, in general, and we all learn continuously through each other. Together, with the staff at HOPE, we have over 100 years’ experience as caregivers and parents. This is why we started HOPE. HBOT cannot help all stroke patients, but it does offer some patients and their families new hope. HBOT can revive brain cells surrounding the stroke-affected area, as is often seen with a SPECT scan (a type of brain image, similar to an X-ray). Whether or not a patient can recover from a stroke depends upon several factors, one of which is the extent and size of the damaged area (similar to an atom bomb blast, there is an area that is not so heavily damaged and the central core). The farther a section of the brain is from the central core, the less likely it is to be impaired. Between the damaged tissue and the unaffected, normal brain is another zone referred to as the penumbra. This important area is another factor in determining how much of a recovery the patient can make. That is because the penumbra contains so-called “dormant,” or “idling,” neurons, brain cells that are nonfunctional but intact. If these cells can be awakened, the patient has a good chance of recovering at least some function. Get in touch with us, let us know how we can help, and join the community, so you can learn more about HBOT and the people who are using it now.
Why aren’t more doctors prescribing HBOT, if accepted by so many hospitals?
Basically, most doctors are not yet familiar with hyperbarics. Also, the use of HBOT involves the expense of installing hyperbaric chambers and hiring the technical staff to run them. Another reason is that HBOT is not year a fully established subject in medical schools. In the US, only forty-six medical schools teach hyperbaric medicine or have hyperbaric chambers. Currently, hyperbaric chambers are being installed in a small number of ambulances throughout the US. Thus, medical students often do not learn about hyperbarics, even though first responders and emergency medicine technicians are adopting hyperbarics at a quick pace. Practicing doctors don’t learn about HBOT because much of their continuing education comes from the pharmaceutical industry, which naturally has no interest in informing doctors about a product it does not sell. Furthermore, it is characteristic of the medical establishment, as with any establishment, to be disposed toward preserving the existing order. If a doctor should become interested in HBOT, he or she must spend a considerable amount of time and effort to search the medical literature for information about this subject. At HOPE, we’re trying to make it easier for interested practitioners to learn more about HBOT.
How do we know if HBOT is working?
A number of imaging systems exist (like SPECT and PET scans) that doctors use to monitor the progress of HBOT. SPECT is particularly useful in following the progress of patients treated with HBOT. Like other body-imaging systems, SPECT causes minimal discomfort for the patient, and, with the use of a tracer, shows the viewer where the active neurons are. Before-and-after scans, in certain instances, show a large region of potentially recoverable brain tissue. Practicing neurologists are slowly coming to agree with the idea of identifying stroke-affected brain tissue that might be recoverable. It is accepted medical practice that every measure should be taken to help awaken the dormant neurons with the damaged tissue and thus restore each patient to as much of that individual’s pre-stroke capacity as possible. The use of HBOT as part of a comprehensive treatment plan is the simplest and most effective way of doing just that.
Is HBOT effective for head injury and concussions?
In some cases, depending on the size and location of the initial damage, as well as the reversibility of the damage within the penumbra, the damage can be reversed by HBOT. Head injury isn’t the only cause of brain damage. Every year, thousands of Americans suffer brain damage as the result of near-hanging, near-drowning, near-choking, concussions from sports, cardiac arrest, cyanide and carbon monoxide poisonings, and lightning strikes. This type of brain damage is known as anoxic ischemic encephalopathy. Simply put, HBOT can help get oxygen to the injured brain. For spinal cord injury patients, HBOT aids by reviving nerve cells in the spinal cord in the same way it can help stimulate nerve cells in the brain.
Similarly, HBOT can assist in the alleviation of migraine headaches, and in the treatment of various eye and ear problems. HBOT can increase oxygen levels, because the increased pressure forces oxygen into the blood plasma, the liquid part of the blood that normally does not carry oxygen, and into the cerebrospinal fluid that surrounds the brain. The plasma and cerebrospinal fluid (CSF) can then reach areas that the red blood cells, which normally carry oxygen, cannot penetrate. With HBOT, oxygen in the capillaries is pushed further into the adjacent tissues than when oxygen is administered at standard pressure. HBOT can also stabilize and repair the blood-brain barrier, the protective layer of cells that keeps many toxins or noxious materials from reaching the brain; this barrier is often greatly disturbed when a head injury occurs. As a result of the extra oxygen that HBOT provides, the dormant brain cells in the penumbra are awakened and begin to function again. Giving patient pure oxygen at normal pressure simply cannot put enough oxygen into either the bloodstream or the CSF to overcome the oxygen deficit. In certain cases, HBOT also allows the patient to recover from brain-damage aftereffects such as paralysis and speech loss.